
Debunking the Fake News of EMRs
The Current EMR Perception
If you are monitoring the healthcare media these days, there is a disturbing number of reports vilifying the EMR as being unusable and driving physician burnout. How much of this is sensational journalism written to grab eyes? What is the current reality? The KLAS Arch Collaborative EMR usability and clinician satisfaction research was initiated to delve into the challenges facing EMR use.
No one can dispute that the EMR has failed to meet expectations established in works such as, Paper Kills - Transforming Health and Healthcare with Information Technology. EMRs were to be the facilitators of high-quality and low-cost healthcare that would drive improved care-delivery outcomes and patient safety. The EMR was also supposed to drive higher levels of patient and clinician satisfaction.
What happened? Well-intentioned academics implemented Meaningful Use (MU). The availability of big money from the government drove many healthcare providers to select and implement EMRs that met the necessary functional requirements and supported quality-outcomes reporting that was tied to reimbursement.
Very few provider organizations created EMR-implementation strategies for the MU-funded EMRs that extended to supporting care delivery. This resulted in EMR implementations that supported billing and coding processes. Clinicians were transformed into data-entry clerks, and the EMRs provided very little return value to the clinicians for improving care delivery.
Yes, the EMR has been a disappointment at best.
But KLAS wanted to find out if providers were as unhappy as the media made it appear, and what provider organizations could do to make the best of their EMRs. To date, nearly 100 provider organizations worldwide have sought end-user feedback about using the EMR. The results were shocking, to say the least:
Arch Collaborative EMR Research Findings
Shocker #1: Many of the fixes needed to improve EMR usability and clinician satisfaction are not technical!
EMR satisfaction has a strong correlation to three key findings: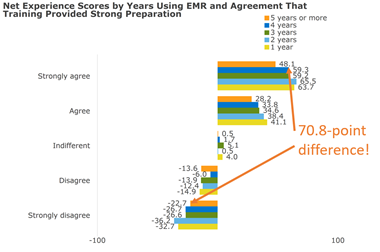
- The Initial EMR training and follow-up education clinicians receive establishes a solid foundation for success that retains high levels of clinician satisfaction over several years.
- The more clinicians use EMR-personalization tools to support their care-delivery workflows, the more satisfied they are. Most organizations tend to focus on the EMR personalizations that facilitate inputting data efficiently—in other words, settings that make clinicians great data-entry clerks.
Ensuring that clinicians receive appropriate personalization training for efficiently extracting patient data results in higher EMR satisfaction. Wasn’t ease of access to patient data a key promise of the EMR’s potential?
- The factor with the highest impact on clinician satisfaction is the organization culture, which is the foundation for EMR governance. How many times does an organization tell a clinician “No” instead of “Let’s discuss some potential solutions”? If clinicians feel that the leaders aren’t listening, they give up and EMR satisfaction goes down the drain. An additional governance frustration is having each change/enhancement request go through multiple approval committees. This pattern results in requests taking six months to two years to be approved.
Shocker #2: The AMA may not have the full story; the EMR is not the key factor in physician burnout.
The Arch Collaborative findings show that over 90% of clinicians either agree or strongly agree that they feel fulfilled in their profession, but many fulfilled clinicians have low EMR satisfaction scores. This indicates that the EMR may be a convenient “whipping boy” for those seeking to solve clinician burnout. Placing all the blame on the EMR means we may fail to consider other professional and lifestyle factors that are driving burnout.
This is not to say that a poorly implemented, supported, or designed EMR doesn’t contribute to physician burnout, but EMRs should be appropriately reviewed as one of many potential factors, instead of the smoking gun.
Shocker #3: Provider organizations in which most clinicians are satisfied with the EMR do exist.
This is the most exciting part of the Collaborative research. We get to expose provider organizations who have some of the best practices. KLAS’ research found high EMR-satisfaction scores at some large healthcare systems, medium healthcare systems, community hospitals, county hospitals, and ambulatory care groups.
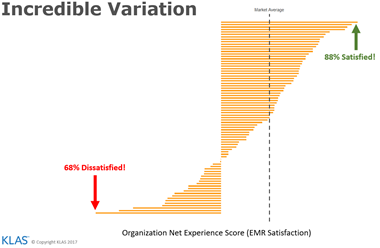
Shocker #4: All of the major EMR vendors have some highly satisfied customers and some highly unsatisfied customers.
The Collaborative research is not a blood sport for identifying the best EMR vendors. The research shows that any organization that focuses on items 1–3 from Shocker #1 can improve their providers’ EMR satisfaction.
Shocker #5: International organizations have similar EMR challenges.
Collaborative members from the UK and Australia (with more countries to follow soon) are validating many of the same EMR challenges and opportunities for improvement that we find in the US.
What’s Next?
The Arch Collaborative is open to all provider organizations, and the first round of participation in the Arch Collaborative is free. A key benefit of the Arch Collaborative is that providers are compared to three cohorts: other Collaborative members, organizations with the same EMR, and organizations of the same size or type. This provides an unparalleled perspective for EMR performance for participating members. The Arch Collaborative team conducts a data review of key findings with the organization after data collection and analysis are completed.
Organizations that want to drive EMR improvement globally can become Collaborative members and participate in the annual benchmarking surveys. The follow-up surveys will compare past and new findings to determine whether improvement efforts have achieved the desired outcomes.
Membership in the Collaborative also includes:
- Access to monthly webinars conducted by Collaborative members who have demonstrated impactful EMR practices.
- Access to a library of case studies of successful EMR use and support, member-requested teleconferences with high-performing member organizations.
- Collaboration with EMR vendors.
- An invite to the annual Arch Collaborative Conference. The first conference will be in Salt Lake City on May 23, 2018.
It is time to rid the industry of “fake news” regarding the EMR. Join the Arch Collaborative and help us realize the original promise of the EMR.